M.D. Anderson study called potential ‘game-changer’ for treating pancreatic cancer
M.D. Anderson researchers may be able to catch pancreatic tumors early
Researchers at M.D. Anderson Cancer Center believe they have found a path to early detection that could yield more effective treatment of pancreatic cancer, an illness so lethal that just 7 percent of patients survive for five years after their diagnosis.
In a study published in Wednesday’s issue of the science journal Nature, the researchers found patients with pancreatic cancer had certain particles in their bloodstream not found in healthy patients or in those with other types of pancreatic disorders. The presence of those particles could determine, with 100 percent accuracy, who had pancreatic cancer and who did not, the study found.
While the test must undergo more rigorous study before it can be used routinely, it could finally provide a reliable, noninvasive way of finding the cancer before it’s too late to treat it.
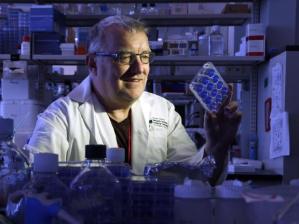
“If it pans out, it’s a game-changer,” said Dr. Raghu Kalluri, chair of cancer biology at M.D. Anderson and a co-author of the study, “and we’re aware that our patients really need that right now.”
The National Cancer Institute estimates 48,960 new pancreatic cancer cases will be diagnosed this year, and it will kill 40,560 people.
Pancreatic cancer has among the worst outcomes of any cancer. The pancreas is located deep within the body, so early tumors cannot be seen or felt, and four out of five patients are diagnosed only after it has spread. Patients usually have no symptoms until the cancer has spread to other organs. While surgery to remove the tumor or entire organ can cure up to 50 percent of early-stage pancreatic cancer, doctors see few patients in that stage.
“It’s almost invariably advanced,” said Dr. Kirk Heyne, a medical oncologist at the Houston Methodist cancer center who was not involved in the study. “Probably 15 percent of people can be taken to surgery.”
‘Unheard of’ accuracy
Even after diagnosis, there are no good ways of tracking what is happening with the cancer. Patients must undergo repeated biopsies or CT scans to determine whether the treatment is working or whether their cancer has progressed or recurred.
Researchers found the marker by looking at exosomes, tiny bundles containing DNA and other genetic material, released by the body’s internal cells.
They compared exosomes from healthy and cancerous cells and found the cancer exosomes contained a particular protein. By searching for exosomes with this protein in the bloodstream, the researchers could detect and quantify the amount of cancer in the body.
They then screened the blood of hundreds of pancreatic cancer patients, diagnosed at different stages, and hundreds of healthy donors for exosomes containing the protein. In addition to M.D. Anderson, institutions in Germany and Spain participated in the study.
“When it was positive for it, it was always in the cancer patients,” Kalluri said, “never in the hundreds of healthy subjects or those who didn’t have pancreatic cancer. The fine difference with which it was able to distinguish is unheard of in the cancer field.”
The test had zero false positive and zero false negative results.
Moreover, the study found the more advanced the patient’s cancer, the more exosomes in their blood, and when tumors were removed with surgery, levels of the exosomes dropped.
Pancreatic cancer experts called the study promising and were eager to see if further research would confirm the accuracy of the test.
“Blood-based biomarker studies for pancreatic cancer have been somewhat disappointing overall,” said Dr. Michael Goggins, director of the Pancreatic Cancer Early Detection Laboratory at Johns Hopkins University. “This one has some promising characteristics.”
The test could be used primarily in patients at higher risk for pancreatic cancer, such as those who are obese, diabetics, smokers or those with a family history of the disease.
(click here to continue reading this article)
*credit verbatim via http://www.houstonchronicle.com *